Diabetic retinopathy can affect individuals living with diabetes, and left unmonitored, can impact eyesight. Regular eye exams are a key part of managing this condition. Understanding what happens during an appointment can help patients feel more prepared. This article addresses what diabetic retinopathy is, what causes it, if wearing contact lenses is a factor, and how it is diagnosed.
What is Diabetic Retinopathy?
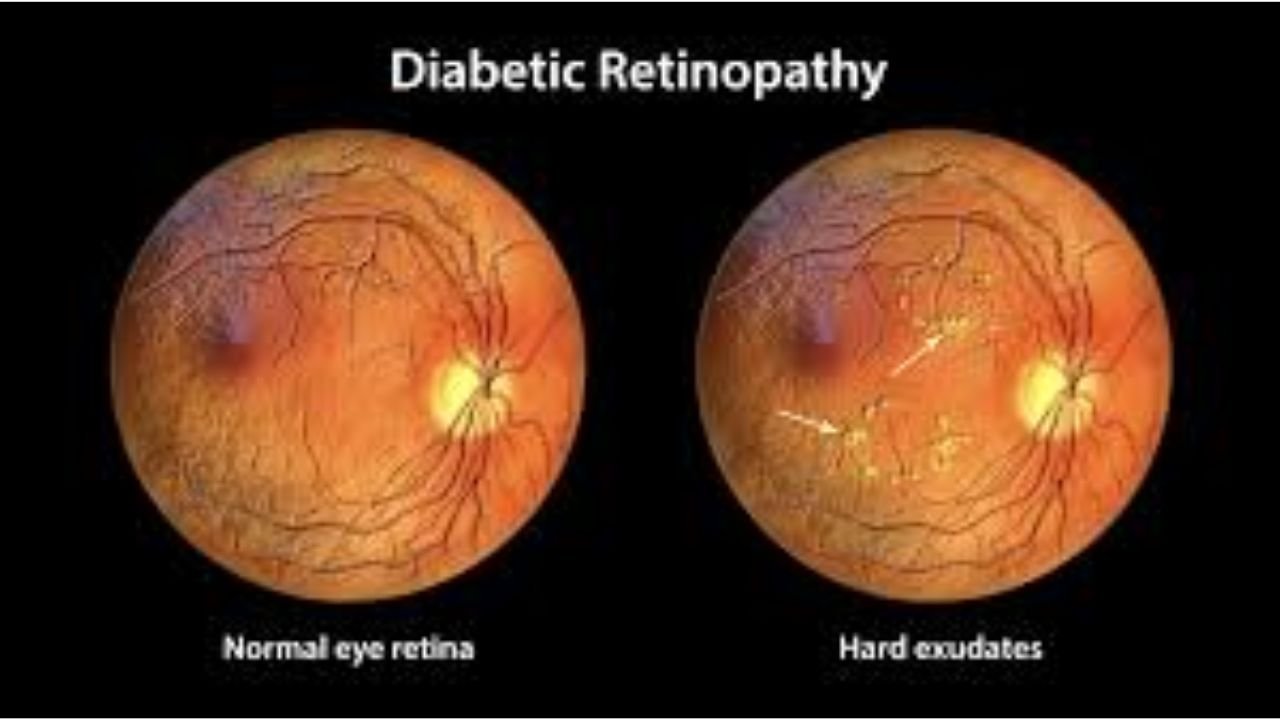
Diabetic retinopathy is an eye condition that occurs when prolonged high blood sugar levels damage the blood vessels in the retina. This condition commonly develops in individuals with diabetes and can progress in stages. Issues can range from mild to more advanced cases involving scarring and changes in vision.
What Causes Diabetic Retinopathy?
Diabetes impacts blood vessels throughout the body, including the capillaries in the retina. High blood sugar levels can weaken these blood vessels, leading to leakage or abnormal growth. Factors such as the duration of diabetes, blood sugar management, and the presence of other conditions can influence the likelihood of developing diabetic retinopathy. Both Type 1 and Type 2 diabetics may experience the condition, making regular eye exams a key practice for maintaining retinal health.
Risks and Precautions With Contact Lenses
Individuals with diabetes who wear contact lenses may have an increased risk of complications. This is due to the altered tear film composition of contact lenses and the potential for reduced corneal sensitivity. These factors can hinder the detection of complications such as infections or microinjuries. Proper lens hygiene and regular follow-ups are key for diabetic lens wearers to minimize risks and monitor eye health.
How Does an Eye Doctor Diagnose Diabetic Retinopathy?
Diagnosing diabetic retinopathy typically involves a comprehensive eye exam. The exam often includes the following steps and tools:
- Dilated Eye Exam: Drops are applied to widen the pupils, allowing the eye doctor to examine the retina and optic nerve more thoroughly.
- Retinal Photography: Specialized imaging captures detailed images of the retina, making it easier to detect small changes in the blood vessels.
- Optical Coherence Tomography (OCT): This advanced imaging technique produces cross-sectional scans of the retina, helping detect fluid buildup or swelling.
- Fluorescein Angiography: This test involves injecting a fluorescent dye into a vein and taking photos of the retina to identify abnormal blood vessel activity.
What Does Your Eye Doctor Look for During the Exam?
During an eye exam for diabetic retinopathy, your eye doctor focuses on specific changes or abnormalities in the eye caused by diabetes. These may include:
- Leaking Blood Vessels: Evidence of blood or fluid leaking into the retina may indicate early signs of the condition.
- Abnormal Blood Vessel Growth: New, fragile blood vessels may form as the retina responds to poor blood supply, which are often hallmarks of advanced diabetic retinopathy.
- Retinal Swelling: A condition known as macular edema, caused by fluid buildup in the central area of the retina.
- Scar Tissue or Vitreous Changes: Scar tissue on the retina or changes within the gel-like fluid inside the eye may signal that diabetic retinopathy has progressed.
How is Diabetic Retinopathy Treated?
While the exact treatment plan for diabetic retinopathy depends on its stage and severity, options are available to slow its progression. Treatments might involve blood sugar management, laser treatments, or medication. Surgery may be advised if advanced stages of the condition occur. Many patients can begin treatment as soon as signs of diabetic retinopathy appear.
Schedule an Eye Exam to Protect Your Vision
Diabetic eye care is part of diabetes management. Regular eye exams play a key role in monitoring the health of your retina and addressing issues early. Staying proactive with your eye care can help maintain your vision and support your overall health. Be sure to contact your eye care provider to schedule your next screening.