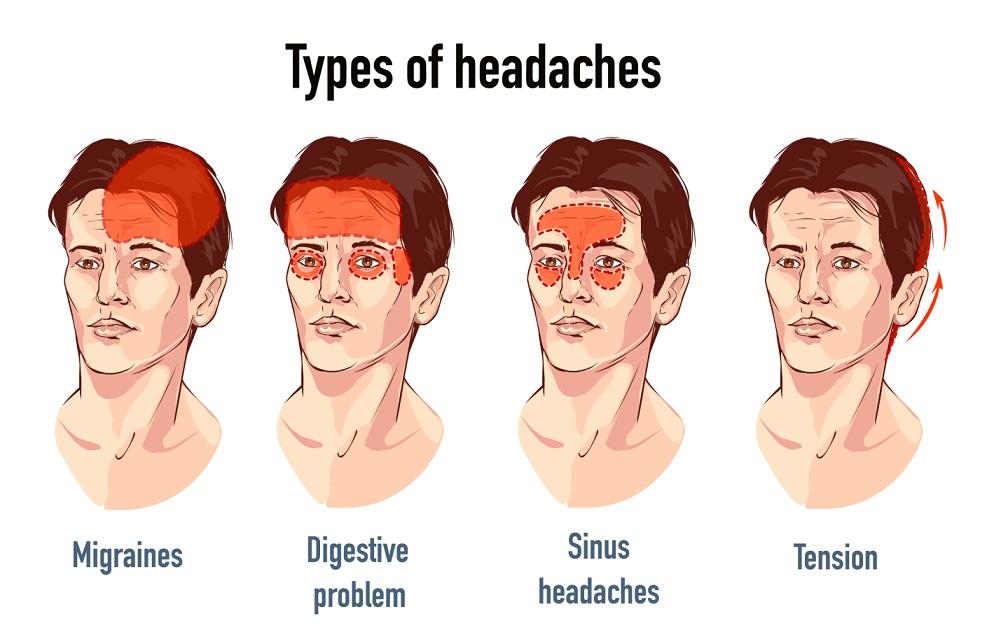
Headaches are one of the most common complaints pain management specialists encounter. Despite being a universal experience, head pain can manifest in various forms, and are uniquely linked to specific triggers and characteristics. Identifying the type of headache patients experience can be the first step in providing effective care. Here is a breakdown of common types of headaches and what may contribute to their occurrence.
1. Tension
A tension headache is one of the most frequently reported types of head pain. They are often described as a dull, aching pain that feels like a tight band around the head. Patients may also report tenderness in the scalp, neck, or shoulders. Potential triggers for this type of headache include:
- Stress: Emotional stress or prolonged focus on a task.
- Posture: Spending extended periods in one position, such as working at a desk, may strain the neck and shoulders, leading to discomfort.
- Sleep Patterns: Irregular sleep schedules or lack of restorative sleep can play a role.
Encouraging patients to adopt stress reduction techniques, ergonomic workspace adjustments, and consistent sleep habits may assist in managing this type of pain.
2. Migraine
Migraines are a complex neurological condition marked by recurring episodes of moderate to severe pain. These headaches are often accompanied by additional symptoms such as nausea, sensitivity to light or sound, and visual disturbances. Common triggers for migraines are:
- Hormonal Changes: Shifts in hormone levels, particularly in women, may correlate with migraine episodes.
- Dietary Factors: Certain foods like aged cheese, chocolate, or processed meats may act as triggers.
- Environmental Triggers: Bright lights, strong odors, or changes in weather can lead to migraines in susceptible individuals.
Understanding individual triggers can help patients better anticipate and manage their migraine episodes.
3. Cluster
Cluster headaches are considered less common than other forms of head pain. They are characterized by intense, sharp pain often localized around one eye. They can occur in groups—or clusters—lasting weeks or even months. Some of the known triggers of cluster headaches include alcohol consumption, high altitude, and exposure to strong odors. Cluster headaches usually follow a predictable cycle, which can assist in diagnosing and preparing potential treatment or avoidance strategies.
4. Secondary
While primary head pains, like those mentioned above, occur independently, secondary headaches are a symptom of an underlying condition. These may be linked to sinus infections, medication overuse, or headaches stemming from head injuries. Detailed patient histories and diagnostic tests often clarify whether a headache is a primary condition or secondary to another issue.
Managing Headache Triggers and Patterns
Encouraging patients to track their head pain through a journal or app can provide valuable insights. They can record information such as food intake, stress levels, environmental conditions, and sleep habits. These logs are excellent tools for identifying patterns and triggers, helping pain management specialists create individualized care plans. Understanding the distinct types of headaches and their potential triggers is key to guiding effective interventions. By fostering awareness of patients’ specific headache patterns and addressing possible contributing factors, pain management specialists are better equipped to provide tailored support.