Mental health treatment is experiencing a revolutionary shift as psychedelic therapy emerges from decades of prohibition into mainstream medical practice. The scientific community has rediscovered what indigenous cultures have known for millennia—certain plant medicines and synthetic compounds possess remarkable healing properties that extend far beyond their immediate effects.
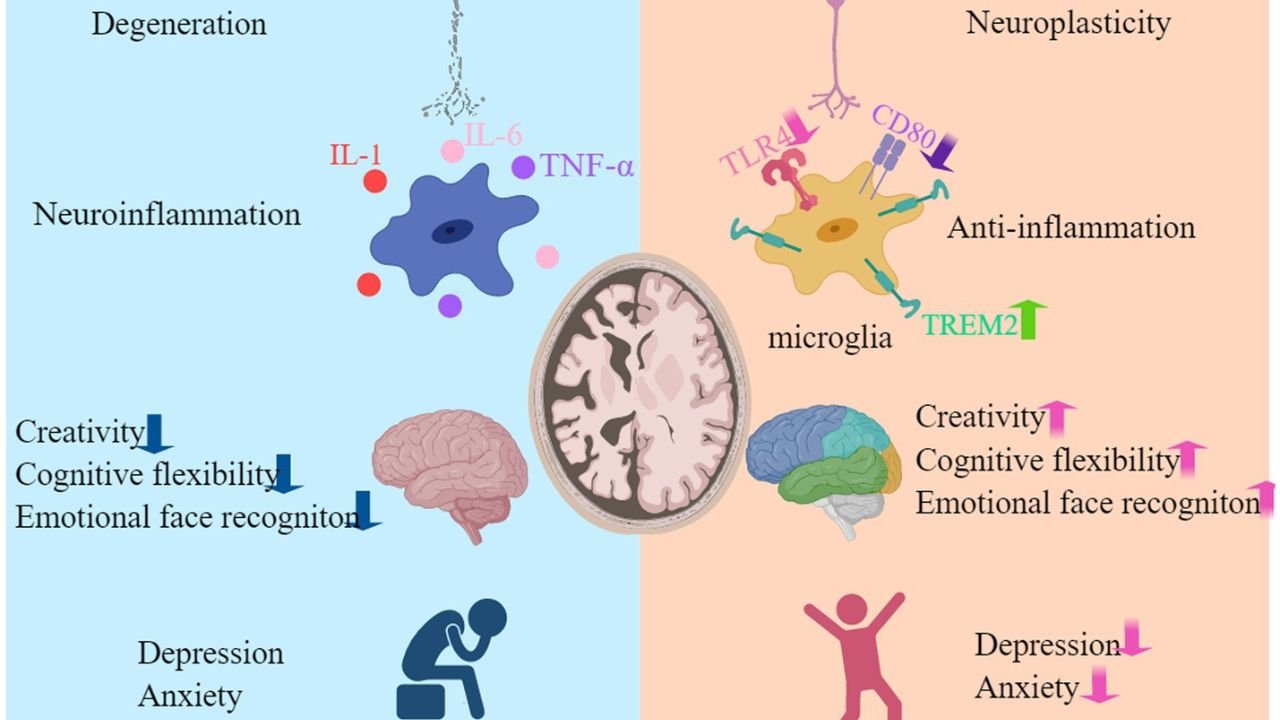
The key to understanding psychedelic therapy lies in neuroplasticity, the brain’s extraordinary ability to reorganize itself throughout life. Unlike traditional psychiatric medications that require weeks or months to show benefits, psychedelic-assisted therapy can catalyze profound changes in brain structure and function within a single session. This breakthrough has opened new pathways for treating conditions that have long resisted conventional approaches.
The Biological Foundation of Healing
Modern neuroscience reveals that mental health disorders often involve rigid patterns of brain connectivity that trap patients in cycles of negative thinking and emotional distress. Breaking free from these patterns requires the brain to develop new neural pathways—a process that psychedelic therapy facilitates with unprecedented efficiency.
Understanding Neuroplasticity
Neuroplasticity represents one of the most significant discoveries in brain science. This biological process allows neural networks to adapt, grow, and form new connections in response to experiences, learning, and therapeutic interventions. When neuroplasticity functions optimally, the brain can recover from trauma, overcome depression, and develop healthier patterns of thought and behavior.
Traditional antidepressants work by gradually encouraging these adaptive changes over extended periods. The process typically requires consistent daily medication for months before patients experience meaningful relief. Psychedelic therapy operates through a fundamentally different mechanism that accelerates neuroplastic changes dramatically.
The therapeutic potential of psychedelics stems from their interaction with serotonin receptors throughout the brain. When these compounds bind to 5-HT2A receptors, they initiate a cascade of molecular events that promote rapid neural adaptation. This receptor activation explains why patients often report lasting improvements that persist long after the psychedelic experience ends.
Molecular Mechanisms of Change
The cellular changes induced by psychedelics involve sophisticated biological processes that support brain health and recovery. Brain-derived neurotrophic factor (BDNF) plays a central role in these mechanisms. This protein functions like fertilizer for neurons, promoting growth, survival, and the formation of new synaptic connections.
Psychedelic therapy significantly increases BDNF production, creating an optimal environment for neural repair and adaptation. The elevated BDNF levels persist for weeks following treatment, providing an extended window during which therapeutic changes can take root and stabilize.
Additional molecular mechanisms contribute to the neuroplastic effects of psychedelics:
- Activation of immediate early genes that respond rapidly to neural activity
- Enhanced protein synthesis supporting synaptic plasticity
- Increased expression of growth factors promoting neural development
- Stimulation of cellular pathways involved in learning and memory formation
Clinical Applications and Therapeutic Mechanisms
The translation of laboratory discoveries into clinical practice has revealed the remarkable therapeutic potential of psychedelic-assisted therapy across multiple mental health conditions. These treatments show particular promise for individuals who have not responded to conventional approaches.
Evidence-Based Treatment Outcomes
Clinical applications of psychedelic therapy demonstrate consistent patterns of neuroplastic enhancement across different conditions and patient populations. Treatment protocols typically involve carefully structured sessions that maximize therapeutic benefits while ensuring patient safety.
The neuroplastic changes induced by psychedelics create lasting structural alterations in brain architecture. Dendritic spines—the tiny protrusions that enable neurons to communicate—show increased density and complexity following treatment. These changes persist for weeks to months, correlating with sustained improvements in symptoms.
Patients receiving psychedelic-assisted therapy often experience breakthroughs that would typically require years of traditional psychotherapy. The enhanced neuroplasticity appears to accelerate the formation of new neural pathways associated with emotional regulation, stress resilience, and adaptive coping strategies.
Comparison with Conventional Treatments
The neuroplastic effects of psychedelics offer distinct advantages over traditional psychiatric medications. While conventional antidepressants require daily administration to maintain their effects, psychedelic therapy can produce lasting benefits following just one to three treatment sessions.
This efficiency stems from the fundamental difference in therapeutic mechanisms. Traditional medications primarily manage symptoms by altering neurotransmitter levels, while psychedelic therapy addresses underlying neural patterns that contribute to mental health disorders. The result is often a more comprehensive and durable recovery.
Key differences between psychedelics and conventional treatments include:
- Duration of treatment: Sessions vs. years of medication
- Mechanism of action: Neuroplastic enhancement vs. symptom management
- Side effects: Temporary vs. ongoing daily effects
- Treatment resistance: Effective for treatment-resistant cases
Brain Network Reorganization
One of the most fascinating aspects of psychedelic therapy involves its effects on large-scale brain networks. The default mode network, which becomes hyperactive in depression and anxiety, shows dramatic changes during and after psychedelic experiences.
Psychedelics temporarily suppress the default mode network while promoting communication between brain regions that typically operate independently. This network reorganization allows patients to break free from rigid thought patterns and develop more flexible, adaptive ways of thinking and feeling.
The suppression of overactive brain networks creates space for healthier neural patterns to emerge. Patients often report reduced rumination, decreased self-criticism, and improved emotional regulation following treatment. These subjective changes correspond to measurable alterations in brain connectivity that persist long after the acute effects subside.
Clinical Implementation and Future Applications
The integration of psychedelic therapy into modern healthcare requires careful attention to treatment protocols, safety considerations, and patient selection criteria. As research continues to validate these approaches, standardized guidelines are emerging to ensure optimal outcomes.
Current Treatment Protocols
Professional psychedelic therapy programs follow structured protocols designed to maximize therapeutic benefits while maintaining safety standards. These programs typically span several weeks or months, incorporating preparation, treatment, and integration phases.
The preparation phase helps patients develop realistic expectations and coping strategies for the psychedelic experience. Therapists assess psychological readiness, address potential concerns, and establish therapeutic goals. This foundation proves critical for achieving positive outcomes and minimizing adverse reactions.
Treatment sessions occur in carefully controlled environments with trained medical professionals present throughout the experience. The setting emphasizes safety, comfort, and therapeutic support rather than recreational use. Patients receive continuous monitoring and guidance to navigate challenging moments and integrate insights as they arise.
Safety Considerations and Patient Selection
Psychedelic therapy requires careful screening to identify suitable candidates and exclude individuals at higher risk for adverse outcomes. Mental health professionals must evaluate psychological stability, motivation for treatment, and potential contraindications before recommending these interventions.
Certain conditions may increase the risk of negative reactions to psychedelic therapy. Individuals with personal or family histories of psychotic disorders require particularly careful evaluation. The temporary alteration of consciousness during treatment can be destabilizing for people with fragile reality testing or severe personality disorders.
Screening protocols typically assess:
- Current psychological stability and symptom severity
- History of psychotic episodes or mood instability
- Motivation and readiness for intensive therapeutic work
- Social support systems and integration resources
Integration and Long-term Outcomes
Psychedelic integration therapy represents a crucial component of successful treatment that helps patients translate insights from psychedelic experiences into practical life changes. The enhanced neuroplasticity following psychedelic therapy creates an optimal window for establishing new behavioral patterns and emotional responses.
Integration sessions typically involve processing the psychedelic experience, identifying key insights, and developing strategies for implementing positive changes. Therapists help patients understand their experiences within the context of their personal history and treatment goals.
The quality of integration support has a significant influence on long-term treatment outcomes. Patients who receive comprehensive integration therapy show greater improvement and more sustained recovery compared to those who lack adequate follow-up care. This underscores the importance of viewing psychedelic therapy as part of a broader therapeutic process rather than a standalone intervention.
Future Research Directions
The field of psychedelic therapy continues to evolve rapidly as researchers investigate new applications, optimize treatment protocols, and develop safer therapeutic approaches. Future studies will likely focus on personalizing treatments based on individual neurobiological profiles and psychological characteristics.
Scientists are exploring whether the neuroplastic benefits of psychedelics can be separated from their consciousness-altering effects. This research could lead to new medications that promote neural adaptation without requiring the intensive supervision currently needed for therapy sessions.
Additional research priorities include understanding optimal dosing strategies, identifying biomarkers that predict treatment response, and developing combination approaches that enhance therapeutic outcomes. These advances will likely expand access to psychedelic therapy while improving safety and efficacy across diverse patient populations.
Summing Up
The science behind psychedelics reveals a profound truth about human neurobiology—the brain possesses an extraordinary capacity for change and healing throughout life. By enhancing neuroplasticity through targeted receptor activation and molecular cascades, psychedelic therapy unlocks this potential in ways that traditional treatments cannot match.
The convergence of ancient wisdom and modern neuroscience has created unprecedented opportunities for treating mental health conditions that have long resisted conventional approaches. As psychedelic therapy moves from research laboratories into clinical practice, it promises to transform not just individual lives, but our entire understanding of what it means to heal the mind.
The future of mental healthcare lies in harnessing the brain’s natural neuroplasticity to create lasting positive change. Psychedelic therapy represents the vanguard of this revolution, offering hope to millions while advancing scientific knowledge of consciousness, healing, and human potential. The age of neuroplasticity-based medicine has begun, and psychedelics stand as its most promising frontier.