Introduction
Can changing what you eat and how you live reduce psoriasis flares? Red meat consumption can increase inflammatory markers like C-reactive protein and interleukin-6, which may be elevated in psoriatic plaques. Alcohol can dilate blood vessels and increase white blood cell production, potentially affecting the skin cell turnover associated with psoriasis. Cold weather can strip moisture from skin while indoor heating reduces humidity, creating conditions that may contribute to plaque development. Understanding these potential mechanisms may help individuals work with healthcare professionals to identify personal triggers and develop appropriate management strategies.
If you’re looking for a psoriasis specialist Singapore to help pinpoint your unique triggers and develop an evidence-based plan, consulting a dermatologist early can make long-term control more achievable.
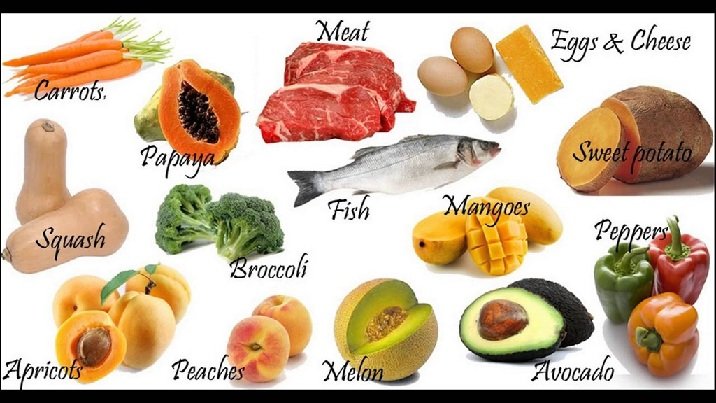
Foods That Trigger Psoriasis Flares
Red Meat and Processed Foods
Red meat contains arachidonic acid, which converts to inflammatory prostaglandins and leukotrienes in the body. These compounds may stimulate the inflammatory cascade associated with psoriatic plaque formation. Processed meats like bacon and sausages contain additional nitrates and advanced glycation end products (AGEs) that may contribute to inflammation.
Fish rich in omega-3 fatty acids, particularly salmon, mackerel, and sardines, provide EPA and DHA, which compete with arachidonic acid for enzyme conversion, producing anti-inflammatory compounds instead. Chicken and turkey contain less arachidonic acid than red meat, making them potential alternatives when consumed in moderation.
Processed foods high in trans fats and refined sugars may trigger insulin spikes that activate inflammatory pathways. Foods with a high glycemic index cause rapid blood sugar elevation, potentially stimulating cytokine production. Whole grains with low glycemic indices, such as steel-cut oats, quinoa, and barley, may be considered as alternatives.
Nightshade Vegetables
Tomatoes, potatoes, peppers, and eggplants contain solanine, a glycoalkaloid that may trigger inflammation in certain individuals with psoriasis. While scientific evidence remains mixed, some patients report improvement after eliminating nightshades.
Consider tracking your response by removing all nightshades completely, then reintroducing one variety every five days while monitoring skin changes. Document flare timing, severity, and specific foods consumed. Some patients tolerate cooked tomatoes but react to raw ones, as cooking reduces solanine content significantly. Consult with a healthcare professional before making significant dietary changes.
Alcohol and Caffeine
Alcohol may disrupt skin barrier function by decreasing filaggrin production and altering ceramide composition in the stratum corneum. Beer and malt beverages contain gluten, potentially problematic for the subset of psoriasis patients with gluten sensitivity. Wine’s histamine content can trigger additional inflammatory responses.
Consider limiting alcohol to special occasions, choosing clear spirits mixed with soda water over beer or wine when consuming alcohol. Space drinks with equal amounts of water to maintain hydration and support liver detoxification pathways.
Caffeine’s effect varies among individuals. While moderate coffee consumption provides antioxidants, excessive intake can disrupt sleep patterns and increase stress hormones. Poor sleep quality may correlate with psoriasis severity, as skin repair processes occur primarily during deep sleep phases.
Daily Habits That Worsen Symptoms
Aggressive Skin Care
Vigorous scrubbing traumatizes psoriatic skin through the Koebner phenomenon, where skin injury triggers new plaque formation at trauma sites. This response typically appears 10–14 days after injury, making the connection easy to miss.
- Pat skin dry with soft towels instead of rubbing.
- Apply moisturizers within three minutes of bathing while skin remains slightly damp to trap moisture.
- Choose fragrance-free products with ceramides, which restore barrier function, over those with alcohol or essential oils that can irritate sensitive skin.
Hot water strips natural oils and disrupts the skin’s acid mantle, worsening dryness and scaling. Keep shower temperature lukewarm, around 35–37°C, and limit duration to 5–10 minutes. Install a shower timer if needed to maintain consistency.
Smoking and Stress
Smoking increases psoriasis risk and treatment resistance. Nicotine promotes keratinocyte proliferation and inflammatory cytokine release while reducing oxygen delivery to skin tissues. Oxidative stress from cigarette smoke damages cellular DNA and depletes antioxidant reserves.
- Consider developing a quit plan with nicotine replacement therapy.
- Varenicline or bupropion may help reduce cravings but require medical supervision.
- Track triggers for smoking urges and develop alternative responses like deep breathing exercises or brief walks.
Chronic stress elevates cortisol and substance P levels, both directly linked to psoriasis flares. Substance P, a neuropeptide, increases during psychological stress and stimulates mast cell degranulation, releasing inflammatory mediators into skin tissue.
Poor Sleep Patterns
Sleep deprivation increases inflammatory markers TNF-alpha and IL-6, key drivers in psoriatic inflammation. Irregular sleep schedules disrupt circadian rhythm regulation of immune function, potentially triggering flares.
- Establish consistent sleep and wake times, varying by no more than 30 minutes even on weekends.
- Create a cooling sleep environment between 18–21°C, as overheating worsens itching.
- Use breathable cotton bedding and sleepwear to minimize skin irritation.
Blue light exposure after sunset suppresses melatonin production, delaying sleep onset. Install blue light filters on devices or cease screen use two hours before bedtime. Replace evening screen time with reading, stretching, or meditation.
Environmental and Physical Triggers
Weather and Humidity
Cold, dry weather increases transepidermal water loss, while low humidity weakens the skin’s natural moisture barrier. Indoor heating systems compound dryness by reducing ambient humidity. In contrast, warm, humid climates can sometimes alleviate scaling but may worsen itching through sweat irritation.
Using a humidifier in dry environments can help maintain 40–50% indoor humidity, reducing flare intensity. Applying occlusive moisturizers like petrolatum or shea butter before bed helps lock in moisture overnight.
Infections and Injuries
Streptococcal throat infections are known triggers for guttate psoriasis. The immune system’s response to bacterial antigens may cross-react with skin proteins, leading to widespread spots on the trunk and limbs.
Skin injuries — even mild ones such as scratches or insect bites — can cause new psoriasis lesions to develop (Koebner phenomenon).
Practicing careful wound care and protecting the skin from sunburn or trauma helps minimize this effect.
Medications That May Trigger Flares
Certain medications can worsen psoriasis or interfere with treatment efficacy, including:
- Beta-blockers (for blood pressure or heart issues)
- Lithium (for mood disorders)
- Antimalarials such as hydroxychloroquine
- Systemic corticosteroid withdrawal, which can provoke rebound flares
Always consult a dermatologist or healthcare provider before stopping or changing any prescribed medication.
What Dermatologists Say
Dermatologists emphasize that psoriasis is multifactorial — dietary and lifestyle factors may worsen or improve symptoms but rarely act alone. Identifying your unique triggers through observation and professional guidance remains the most reliable approach.
A board-certified dermatologist can help determine whether your psoriasis is primarily immune-driven, triggered by external irritants, or linked to metabolic or hormonal imbalances. They can also personalize topical, phototherapy, or systemic treatment options accordingly.
Conclusion
Avoiding common dietary and lifestyle triggers may help reduce psoriasis flare frequency and severity, but each person’s experience differs. Track your own reactions and work closely with a dermatologist to develop a sustainable, evidence-based routine for clearer, healthier skin.